"Research Roundup" September 2024 Edition
- Jennifer Philips
- Sep 30, 2024
- 4 min read
Research Roundup is a monthly newsletter from N of One’s UK-based science writer, Paul Whiteley, PhD. Each month we summarize a few research papers on a variety of topics in one simple, easy-to-read paragraph. It’s our hope that by skimming these each month, you will broaden your knowledge topics currently being explored by researchers and perhaps find information helpful in your journey of navigating a complex autism landscape.

Sulforaphane, autism and gut bacteria
Initial research funded by N of One on the potentially important effects of the compound sulforaphane in relation to autism continues to gather momentum. A recent study from China expanded the research to look at how sulforaphane impacts gut bacteria both in people diagnosed with autism and in animal models. This multilayered approach relied on behavioral and gut microbiome markers, and looked at both animal models (MIA Maternal Immune Activated rats) and a small group of ASD kids. Sulforaphane, an important compound found in cruciferous vegetables such as broccoli with multiple antioxidant, antimicrobial, and anti-inflammatory properties, showed some important effects in both people and animals. Importantly, no serious side effects from sulforaphane dosage were observed in children. Positive behavioral changes were seen in children using sulforaphane and similarly noted in some rat behaviors under experimental conditions. Both children and animals also showed “consistent changes in order Bacillales, family Staphylococcaceae and genus Staphylococcus” indicating a possible mechanism for the behavioral effects observed. Such work stresses a potentially important ‘gut-brain’ connection and implies more study of sulforaphane as a potential autism intervention.
[note from J. Rodakis: research into Sulforaphane was the first we funded, even before N of One was officially formed – glad to see it continue to show promise]
Transcranial magnetic stimulation and autism meta-analyzed
TMS or transcranial magnetic stimulation of the brain appears to have some important evidence of positive effects in relation to autism, concludes a review paper out of China. Part of a growing area of interest into how magnetic fields can be used to stimulate parts of our very electrical brains (or at least nerve cells), such data sets the scene for further study in this important area. Here, 17 studies were included for review, mixing randomized controlled trials and open trials. Various parts of the brain were targets of TMS, also crossing various durations and frequencies of TMS use. Most studies reported some positive changes to recorded symptoms on “stereotypical behavior, repetitive behavior, verbal and social aspects of ASD.” Adverse effects weren’t specifically looked at in this review but authors did allude to other research on this topic suggesting that about a quarter of people with ASD who undergo TMS have minor side-effects such as headaches or dizziness. Overall however, TMS seems to be a fairly safe and well-tolerated intervention option that requires more study on optimal use and importantly, why such effects are noted.

The gut mycobiota and autism: a role for yeasts
To talk about gut bacteria in the context of autism doesn’t really do justice to the variety of other species that inhabit the human gastrointestinal (GI) tract. A new paper from N of One supported collaborators out of Arizona State University refocuses attention on another important ecosystem: the gut mycobiome or the collected yeasts that call the gut home. Looking at the gut mycobiome in some 80 children, half diagnosed with autism and half typically-developing non-autistic controls, researchers observed some interesting trends based on stool analysis for yeasts. The primary finding was that levels of Saccharomyces cerevisiae - otherwise known as brewer's yeast - was significantly lower in samples from those with autism. Likewise, among a proportion of those with autism, overgrowth of Candida albicans was detected, correlating with more severe autism severity according to the Autism Treatment Evaluation Checklist (ATEC) scores also analyzed. Such work adds to a relatively small bank of information in this area. As to what to do about such findings, analysis of the potential usefulness of antifungal medicines and supplements (including use of a relation, Saccharomyces boulardii) needs to be a research priority.
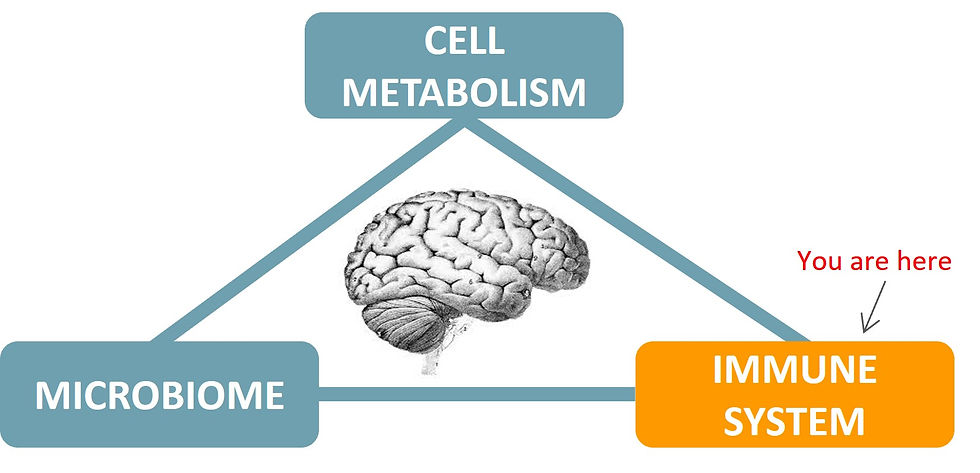
Anti-inflammatory treatments for autism
A research giant in the field of the immune system and autism recently published a comprehensive overview of the potential anti-inflammatory interventions that could be utilized for autism. Harumi Jyonouchi, whose work stretches from looking at primary immune deficiencies to atopic diseases in the context of autism, provides an evidence-based tour de force on the various immune-modulating interventions that currently could be suitable for those diagnosed with autism, specifically targeting inflammatory processes. Alongside reviewing the potential usefulness of various biological interventions, a key point raised in the article is the various ways that clinicians should be screening for immune related issues in the context of autism. Such screening provides important guidance for what intervention(s) may be most suitable and for who.
“28% of patients with first-episode psychosis had a comorbid autism diagnosis”
A new study out of Hong Kong provides further evidence for an important connection between the autism and schizophrenia spectrums. Based on the examination of over a hundred children diagnosed with first-episode psychosis, researchers used one of the gold-standard autism assessment instruments (Autism Diagnostic Interview- Revised, ADI-R) to probe how many children would reach autism cut-off scores. Alongside a quarter of their cohort having been diagnosed with autism, an additional 30% also met the diagnostic cut-off points for autism based on their ADI-R scores. They additionally found that boys were overwhelmingly more likely to have “first-episode psychosis-autism spectrum disorder comorbidity” than girls. Psychosis is a serious condition that can have multiple adverse effects, particularly on children. Such work pinpointing autism as an important part of the clinical picture of many children with psychosis implies preferential screening for autism and offering timely and appropriate intervention options.
Full-text: https://pubmed.ncbi.nlm.nih.gov/38869152/




Comments